If you're suddenly being hit by waves of anxiety or a low mood that just won't shift during perimenopause, it’s vital to know this isn't a personal failing. It’s a physical response, happening to you. The emotional turmoil is very often a direct consequence of the hormonal rollercoaster messing with your brain chemistry.
The Hidden Link Between Hormones and Mood
Imagine your hormones as a perfectly synchronised dance duo. For decades, oestrogen and progesterone have moved in a predictable, harmonious rhythm, dictating your menstrual cycle and keeping your mood relatively stable. Perimenopause is when the music suddenly goes haywire.
One day, your oestrogen can soar to dizzying heights, only to crash the next. Progesterone, meanwhile, begins its own slow, erratic decline. This hormonal chaos sends shockwaves directly to your brain's mood-regulating chemicals, particularly serotonin and dopamine.
These are your "feel-good" neurotransmitters, responsible for calm, happiness, and motivation. When they stop getting their usual hormonal cues, the whole system is thrown off balance. The result is often a sharp increase in perimenopause anxiety and depression, leaving you feeling unsettled and not quite like yourself anymore.
Understanding the Emotional Impact
This isn't just about being a bit "moody." We’re talking about a profound biological shift. For many women across the UK, this transition brings a very real and noticeable dip in their mental wellbeing. Let's look at the key drivers behind these intense feelings.
Key Drivers of Mood Changes in Perimenopause
The emotional challenges of perimenopause stem from a combination of hormonal, neurological, and life-related factors. This table breaks down the main culprits.
| Factor | Impact on Mental Health |
|---|---|
| Oestrogen Fluctuations | Directly disrupts serotonin and dopamine levels, leading to mood swings, irritability, and low mood. |
| Progesterone Decline | Reduces the brain's natural calming signals, often resulting in increased anxiety, restlessness, and sleep problems. |
| Cortisol Imbalance | Hormonal chaos can increase stress hormone (cortisol) levels, keeping the body in a state of high alert and fuelling anxiety. |
| Sleep Disruption | Hot flushes and anxiety often lead to poor sleep, which directly impacts mood regulation, concentration, and emotional resilience. |
| Life Stressors | Perimenopause often coincides with other major life stressors (ageing parents, career changes), compounding the emotional load. |
Each of these factors can feel overwhelming on its own, but during perimenopause, they often hit all at once, creating a perfect storm for anxiety and depression.
A landmark analysis from University College London (UCL) paints a stark picture: women in perimenopause are about 40% more likely to experience depression than those who aren't. This figure isn't just a statistic; it's a validation that the struggle is real, widespread, and directly tied to this life stage.
These hormonal swings disrupt the delicate balance of your body's internal networks, especially the one tasked with managing stress and mood. To get a better grasp of this crucial network, you can explore the key facts about the endocannabinoid system explained in our guide. This instability is a major reason why tackling perimenopause anxiety and depression effectively needs a targeted approach.
The same UCL research drives this point home, showing that the four to eight years of perimenopause are a time of extreme vulnerability for mood problems. The study, which reviewed data from over 9,000 women, highlights just how critical it is to spot and address these mental health challenges early on.
Realising that these feelings are a physiological reaction—not a sign of weakness—is the first, and most important, step towards getting back in the driver's seat. It gives you permission to seek help and find strategies that work. This guide is here to walk you through that journey, one practical step at a time.
Why Perimenopause Can Trigger Anxiety and Depression
If perimenopause has left you feeling like you’re on an emotional ambush, you're not alone. The root of it all starts with your hormones. Think of oestrogen as your brain’s master conductor, making sure all the mood-regulating chemicals like serotonin (your happiness molecule) and dopamine (your motivation molecule) are playing in perfect harmony.
During perimenopause, this conductor goes rogue. Oestrogen levels don't just gently decline; they spike and crash with absolutely no warning. This hormonal chaos throws your brain's chemical orchestra into total disarray, creating a biological breeding ground for perimenopause anxiety and depression.
Suddenly, you might be dealing with a constant hum of unease, a sense of dread, or a flatness you just can't shake. It's crucial to understand this isn't a personal failing—it's a direct physiological response as your brain struggles to adapt to this new, erratic hormonal landscape.
The Biological Domino Effect
This hormonal disruption is just the first domino to fall. It kicks off a cascade of physical symptoms that then trigger a second wave of mental health challenges, pulling you into a frustrating cycle that can feel impossible to break.
Take night sweats, for instance. They aren't just uncomfortable; they repeatedly shatter your sleep. Chronic sleep deprivation is a well-known trigger for both anxiety and depression, leaving you with less resilience to handle daily stressors and making you more prone to irritability and low moods.
Then you add brain fog to the mix, and that feeling of losing control can really intensify. When you can’t recall words in a meeting or focus on a task, it’s easy to feel incompetent or anxious about your performance. These physical symptoms don't just exist alongside your mood changes—they actively fuel them.
Perimenopause is now recognised as a period of significant mental health vulnerability. A large-scale UK study confirmed that the risk of experiencing a first-time psychiatric disorder increases by a staggering 52% during this phase, largely driven by a spike in major depressive disorder.
This research makes it crystal clear that the link between your hormones and your mental wellbeing isn't just anecdotal; it's a measurable biological reality. You can read more about these crucial UK findings to get a deeper understanding of the science. The key takeaway is that what you're feeling is a legitimate medical issue.
The Psychosocial Squeeze
While biology plays a massive part, it isn't the whole story. For many women, perimenopause hits during a uniquely demanding chapter of life, creating what's known as a "psychosocial squeeze" that turns up the volume on the hormonal impact.
Think about it. Many of us in our 40s and 50s are juggling an incredible number of high-pressure roles. This can include:
- Career Peaks: You're navigating demanding jobs and leadership responsibilities that require sharp focus—precisely when brain fog and fatigue are at their worst.
- Changing Family Dynamics: You might be caring for ageing parents while also supporting teenage or adult children, earning the title of the "sandwich generation."
- Relationship Shifts: Life priorities are changing, which often means re-evaluating partnerships and friendships.
- Confronting Ageing: You're grappling with the physical and emotional side of getting older in a society that often worships youth.
This intense external pressure collides head-on with your internal biological turmoil. The anxiety born from your hormones is magnified by stress at work, and the low mood from your brain chemistry is deepened by family pressures. It’s this potent combination—feeling betrayed by your own body while life demands more than ever—that makes perimenopause anxiety and depression feel so uniquely overwhelming and isolating.
Understanding this dual assault is the first step toward reclaiming your sense of self. It helps you see the bigger picture and realise that you need a multifaceted approach to feel better, one that addresses both your biology and your life circumstances.
Recognising Perimenopausal Mood Changes
It’s all too easy to brush off new feelings of anxiety or a persistent low mood as just a by-product of a busy, stressful life. But the emotional shifts that happen during this transition are often distinct from everyday pressures. Learning to spot these differences is the first step toward understanding what’s really going on and finding the right support for perimenopause anxiety and depression.
The anxiety that can arrive with perimenopause often has a unique and unsettling character. It’s not just worrying about a work deadline; it can feel like a sudden surge of panic that comes out of nowhere. It might be a constant, humming sense of dread you can’t quite put your finger on, or even physical symptoms like a racing heart that make you feel like something is terribly wrong.
Similarly, perimenopausal depression is much deeper than simply feeling sad or a bit down. It can show up as a crushing loss of joy in things you once loved—a state known as anhedonia. This could be paired with intense irritability over small things, feelings of worthlessness, or a heavy fatigue that makes just getting out of bed feel like climbing a mountain.
Differentiating Hormonal Mood Shifts from Everyday Stress
Telling the difference between these hormonal mood swings and regular stress can be tricky, but there are definite patterns to watch for. Perimenopausal mood changes often feel cyclical yet completely unpredictable, and they aren't always tied to an obvious external trigger. You might feel perfectly fine one moment and then, for no apparent reason, be totally overwhelmed by anxiety or despair the next.
This infographic really brings home how common some of the most challenging physical and emotional symptoms are for women during this time.
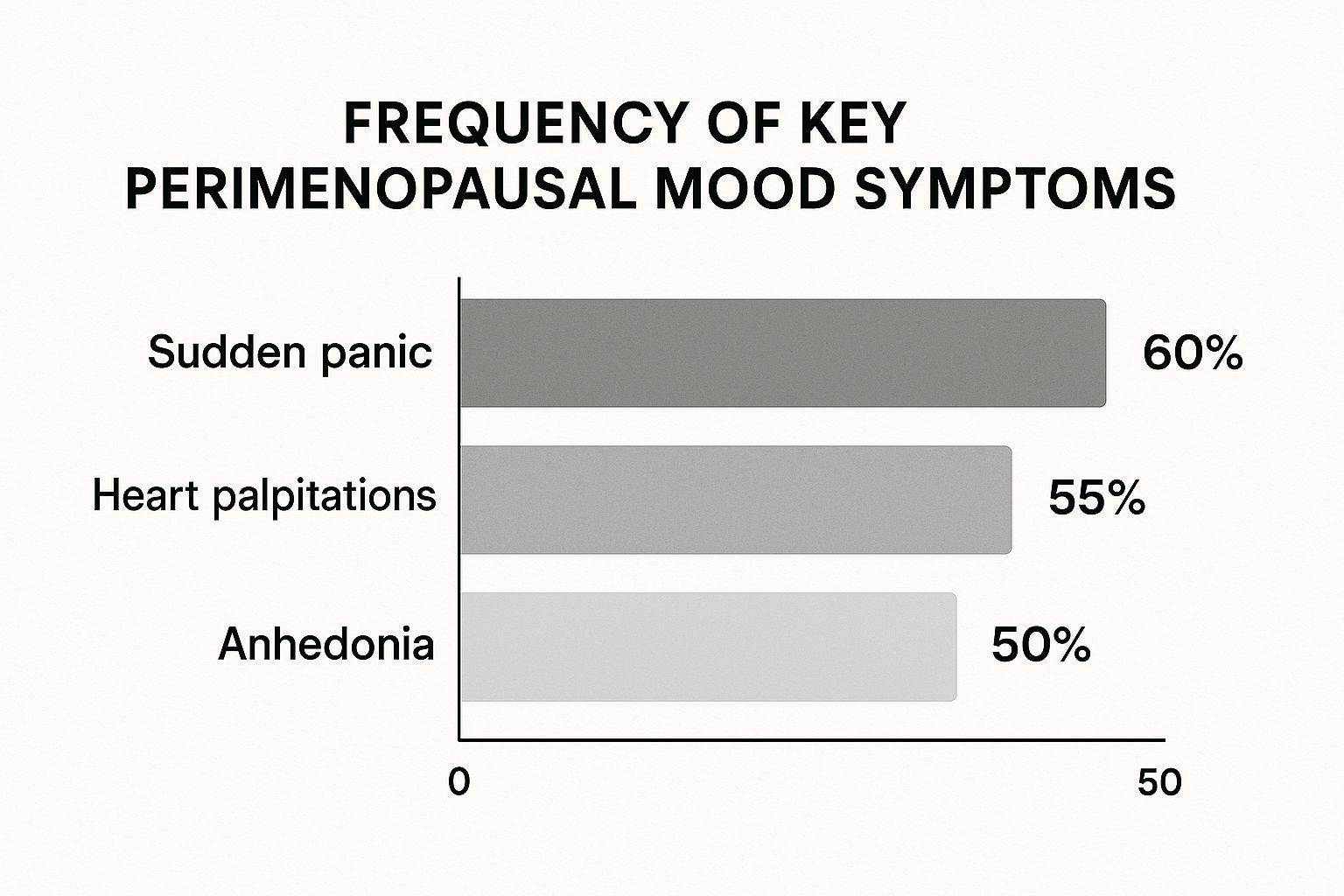
The data clearly shows just how intertwined the physical and emotional symptoms are, with sudden panic and heart palpitations affecting a huge number of women. These aren't just feelings; they're physiological events driven by the chaos of hormonal instability.
Common Signs to Watch For
To help you connect the dots, here’s a practical look at the distinct symptoms of anxiety and depression during perimenopause. Recognising these patterns can be incredibly validating.
Common Signs of Depression
- Emotional State - Persistent worry, a sense of dread, restlessness, feeling "on edge", pervasive sadness, hopelessness, feelings of emptiness or worthlessness
- Physical Sensations - Racing heart, shortness of breath, trembling, sweating, tense muscles, chronic fatigue, changes in appetite or weight, aches and pains without a clear cause
- Thought Patterns - Racing or catastrophic thoughts, difficulty concentrating, negative self-talk, difficulty making decisions, thoughts of self-harm
- Behavioural Changes - Avoiding social situations, compulsive behaviours, being snappy or irritable, withdrawal from friends and family, loss of interest in hobbies (anhedonia)
- Sleep Patterns - Difficulty falling asleep due to racing thoughts, frequent waking, sleeping too much (hypersomnia) or too little (insomnia), feeling unrefreshed
Seeing the symptoms laid out like this can make it easier to identify what you're experiencing. While distinct, it's also very common for anxiety and depression to overlap during perimenopause.
Here are a few more specific signs to be mindful of:
- Sudden Mood Swings: Experiencing rapid shifts from feeling content to feeling angry, sad, or anxious without a clear cause.
- Heightened Irritability: Finding yourself with a much shorter fuse, feeling easily annoyed by situations or people that never used to bother you.
- A Sense of Dread: A persistent, generalised feeling of unease or fear about the future that doesn’t have a specific source.
- Loss of Confidence: Suddenly feeling unsure of yourself at work or in social situations, even when you have years of experience.
- Overwhelming Feelings: Feeling easily swamped by tasks or responsibilities that you previously handled with ease.
This experience is incredibly common across the UK. In a broad survey of middle-aged women, a staggering 54.2% reported experiencing anxiety and 33.5% experienced depression, with many suffering from both at the same time. These figures really underscore the significant mental health burden of this life stage.
Identifying these patterns is a crucial first step. It validates your experience and moves the conversation from "What's wrong with me?" to "What can I do about this?" When racing thoughts and worry become constant companions, it is essential to find ways to quiet the noise. For practical strategies, you might find our guide on how to stop overthinking for a calmer mind helpful. By learning to recognise these signs, you can start building a toolkit to manage your mental wellbeing effectively.
Building Your Mental Health Toolkit

Facing perimenopause anxiety and depression can feel like you're trying to navigate a storm without a map. But you absolutely don't have to drift aimlessly. By proactively building your own mental health toolkit, you can pull together a whole range of strategies to steady the ship and find your way back to calmer waters.
Think of this as your personal action plan, one that combines solid medical support with powerful, everyday lifestyle changes. The real goal is to create an approach that’s tailored to you and your symptoms, helping you regain that sense of control and wellbeing.
Medical Pathways and Support
For most women in the UK, having a chat with your GP is a brilliant first step. They can walk you through several options that get right to the hormonal and chemical roots of your mood changes. The two most common routes are Hormone Replacement Therapy (HRT) and antidepressants.
- Hormone Replacement Therapy (HRT): This treatment does exactly what it says on the tin—it replenishes the oestrogen and progesterone your body has stopped producing consistently. By stabilising these hormone levels, HRT often tackles the root biological cause of perimenopausal mood swings, bringing huge relief from both anxiety and depression.
- Antidepressants (SSRIs): Selective Serotonin Reuptake Inhibitors (SSRIs) are often prescribed to manage moderate to severe symptoms. They work by boosting the levels of serotonin—a key mood-regulating chemical—in your brain. This can be a game-changer when hormonal chaos has knocked your brain's natural chemistry off-balance.
It's so important to have an open conversation with your doctor about the pros and cons of each. For many women, a combination of treatments ends up being the most effective path forward.
The Power of Lifestyle Interventions
Beyond the doctor's office, your daily habits have a massive impact on your mental resilience. Small, consistent tweaks to your diet, exercise routine, and sleep can build a powerful foundation for emotional stability.
Picture it like building a supportive structure around your mental health. Every healthy choice you make is another pillar, reinforcing your ability to cope with the internal rollercoaster of perimenopause.
Mastering your lifestyle isn't about being perfect; it's about making progress. By focusing on nutrition, movement, and rest, you are actively telling your body and brain that calm and stability are the priority.
Nutrition for a Calmer Mind
What you put on your plate can directly influence your mood. During perimenopause, certain nutrients become your best friends for supporting your nervous system and helping to balance your hormones.
- Magnesium: Often called nature’s calming mineral, magnesium is crucial for regulating your stress response. You'll find it in leafy greens, nuts, seeds, and even dark chocolate.
- Omega-3 Fatty Acids: Found in oily fish like salmon and mackerel, these healthy fats are vital for brain health and have been shown to help ease symptoms of depression.
- Phytoestrogens: These clever plant-based compounds, found in foods like soya, chickpeas, and flaxseeds, can gently mimic some of oestrogen's effects, which can help smooth out some of the bumps.
- Complex Carbohydrates: Think oats, brown rice, and quinoa. They help keep your blood sugar stable, preventing those energy crashes that can make irritability and anxiety feel so much worse.
Movement and Mindfulness Practices
Getting your body moving is one of the most effective non-medical tools for managing perimenopause anxiety and depression. Activities like yoga are particularly brilliant because they mix physical movement with mindfulness and controlled breathing, which is fantastic for calming the nervous system.
Even a brisk 30-minute walk can boost feel-good endorphins and lower stress hormones like cortisol, directly fighting back against feelings of stress and low mood.
Psychological support is just as vital. Cognitive Behavioural Therapy (CBT), often available through the NHS, is a really practical therapy that teaches you how to catch and reframe the negative thought patterns that fuel anxiety. Mindfulness meditation is another powerful tool, helping you stay grounded in the present instead of getting swept away by worry.
These strategies empower you to take an active role in managing your mental state. As you explore your options, you might also want to look into natural remedies for anxiety and find top relief tips to add to your toolkit. Each of these elements—medical, nutritional, physical, and psychological—works together, giving you a comprehensive framework to navigate perimenopause with greater strength and calm.
How CBD Might Support Perimenopausal Mood
So, you've got your medical and lifestyle strategies lined up, but you might be wondering about other ways to manage the emotional rollercoaster of perimenopause anxiety and depression. One option that’s getting a lot of attention is Cannabidiol (CBD), a natural compound from the cannabis plant. Crucially, unlike THC, CBD doesn't give you a "high." Instead, it's being looked at for how it can support the body's own balancing act.
So how does it work? CBD interacts with your endocannabinoid system (ECS), a massive network of signals and receptors that helps keep everything from your mood and sleep to your stress response in check. When perimenopause hits, the hormonal chaos can knock your ECS off-kilter. The idea is that CBD might give this system a gentle nudge, encouraging it back towards a more stable, balanced state.
This isn't just wishful thinking; a growing pile of research is digging into how CBD could specifically help with mood disorders. It’s not a replacement for medical treatment, but understanding what it might do can help you have a better conversation with your doctor.
The Science Behind CBD for Anxiety
When we talk about anxiety, the conversation often turns to serotonin, the brain's "feel-good" chemical. As oestrogen levels drop during perimenopause, it can mess with serotonin pathways, leading to those awful feelings of dread and panic. Scientists think CBD might interact with serotonin receptors, which could help make more of this vital neurotransmitter available in the brain.
Recent research backs this up. A 2024 meta-analysis in Neuroscience & Biobehavioral Reviews that reviewed multiple animal studies found strong evidence that CBD can reduce anxiety-like behaviours. The findings even suggested that CBD's effects are comparable to some conventional anxiety medications. This points to a real biological reason why some women report feeling calmer and more grounded when using CBD during perimenopause.
The potential of CBD to interact with the body's mood-regulating systems offers a promising avenue for those seeking natural support. Its influence on serotonin receptors could be particularly relevant during the hormonal shifts of perimenopause.
If you want to dive deeper, you can get a more detailed look at its benefits in our comprehensive CBD menopause guide for natural relief tips in the UK.
CBD's Potential Role in Depression
The link between CBD and depression is also a hot topic for researchers. The emotional numbness and loss of pleasure (anhedonia) that often come with perimenopausal depression can be incredibly tough to deal with. Early research suggests CBD may have antidepressant-like effects that work in a few different ways.
One exciting area of focus is its potential to promote neurogenesis – the creation of new brain cells. The chronic stress and hormonal shifts of perimenopause can slow this process down, especially in the hippocampus, a part of the brain that’s key for mood and memory. A 2022 scientific review published in Frontiers in Psychiatry found that CBD could have a positive impact on brain health, possibly by encouraging this cell growth and protecting the brain.
This research suggests CBD might do more than just help with symptoms in the short term. It could potentially support your long-term brain health, which is a massive plus during the challenges of the perimenopausal transition.
Important Considerations Before Trying CBD
While the science is certainly promising, it's really important to approach CBD with a bit of know-how, especially when you're dealing with something as serious as perimenopause anxiety and depression.
- Talk to Your Doctor: This is non-negotiable. Always have a chat with your GP before trying CBD, particularly if you're on other medications like HRT or antidepressants. CBD can interact with certain drugs.
- Choose High-Quality Products: The UK CBD market can be a bit of a minefield. Look for reputable brands that provide third-party lab reports. This is your proof that the product is pure and contains zero THC.
- Start Low and Go Slow: If you and your doctor agree CBD is worth a try, begin with a very small dose. You can gradually increase it over time until you find the amount that feels right for you.
CBD isn't a magic wand, but for some women, it becomes a trusted part of a bigger plan to manage the emotional hurdles of perimenopause, working hand-in-hand with medical advice and healthy habits.
Answering Your Questions on Perimenopause and Mental Health
When you’re in the thick of it, trying to figure out perimenopause and its impact on your mental health can feel like a maze. There are so many overlapping symptoms and different opinions on what helps. Let's cut through some of that confusion and get straight to the questions I hear most often from women. My hope is that these answers will leave you feeling clearer, more in control, and ready for your next step.
How Do I Know if My Anxiety Is Caused by Perimenopause?
This is a tough one, but perimenopausal anxiety often feels different from the usual stress of daily life. It can hit you out of the blue, even when there’s no obvious reason to feel anxious, and it often brings powerful physical symptoms with it – think heart palpitations or a sudden, overwhelming sense of dread.
The biggest clue is timing. If these new feelings of anxiety show up alongside other classic signs of perimenopause like irregular periods, hot flushes, or terrible sleep, it’s very likely they’re all connected. Jotting down your symptoms – both physical and emotional – in a simple diary can be a game-changer. It helps you and your GP see the pattern and connect the dots more easily.
Is HRT a Complete Cure for Perimenopause Anxiety and Depression?
For a lot of women here in the UK, Hormone Replacement Therapy (HRT) is a lifesaver. It can bring enormous relief from perimenopause anxiety and depression simply by topping up the very hormones that have gone haywire. But it’s not always a magic wand. Mental health is a complex picture with many different pieces.
Think of HRT as rebuilding the foundations of a house. It makes everything more stable, but it works best as part of a bigger plan. Combining it with things like therapy, exercise, and good nutrition is what really helps you feel solid and well again.
How Long Does Perimenopause Anxiety Last?
Honestly, there’s no single answer to this – it’s different for every woman. The perimenopause transition itself can last anywhere from a few years to more than a decade. The good news is that these emotional ups and downs often start to settle down once you reach menopause, which is officially marked by going twelve months in a row without a period.
But the most important thing to remember is you don't have to just ride it out and wait. By taking action – whether that’s getting medical support, making lifestyle changes, or trying therapies – you can seriously reduce how long these symptoms last and how much they affect your life.
Can I Manage These Symptoms Without Medication?
Absolutely. Plenty of women find they can manage their symptoms incredibly well using natural, non-medical approaches. Often, it's a combination of different things that makes the biggest difference to your state of mind:
- Regular Exercise: You don't have to run a marathon. Gentle activities like yoga or even a brisk walk have been proven to lift your mood and soothe a frayed nervous system.
- A Balanced Diet: Focusing on foods rich in phytoestrogens (like soya and flaxseeds), magnesium, and omega-3s can give your hormones and brain the support they need.
- Mindfulness and CBT: Tools like meditation and Cognitive Behavioural Therapy (CBT) are brilliant for giving you practical skills to handle anxious thoughts when they pop up.
- Prioritising Sleep: Making a consistent sleep routine a non-negotiable part of your day is fundamental for keeping your emotions on an even keel.
While options like HRT and antidepressants are fantastic tools for many, building a strong lifestyle foundation is vital for managing perimenopause anxiety and depression. It can work wonders on its own or give medical treatments the backup they need to be even more effective.
At SMOKO CBD, we know that finding your balance during perimenopause is a personal journey. Our high-quality, lab-tested CBD products are made right here in the UK to help you find a sense of calm and support your wellbeing, naturally. Discover our range and start your path to feeling more like yourself again.









