Getting an autoimmune diagnosis can feel like the ground has shifted beneath your feet. It fundamentally changes the conversation you have with your own body and how you look at the future. Living with an autoimmune disease isn't just about managing symptoms; it's a journey of learning, adapting, and finding a new way to thrive. It's about moving from being a passive patient to the active, hands-on manager of your own health.
Your Journey with Autoimmune Disease Starts Here

Welcome. If you're here, you're looking for more than just clinical information—you're looking for understanding. We get that a diagnosis is so much more than a medical label; it's a profound shift in your daily reality. This guide is designed to be your companion, offering clarity and genuine support for the road ahead.
Think of your immune system as a fiercely loyal guard that's suddenly become confused, mistaking your own body for an intruder. It’s a classic case of friendly fire, where the very system built to keep you safe is now causing harm. This internal mix-up is at the heart of the wide-ranging, and often invisible, symptoms you might be experiencing.
A Path Forward with Support and Strategy
If your diagnosis has left you feeling isolated, please know you are far from alone. These conditions are much more common than people realise. A huge UK-based study involving 22 million people revealed that approximately 1 in 10 individuals now lives with an autoimmune condition. It's a significant and growing health challenge, and you can read the full findings from The Lancet study on the rising incidence of autoimmune diseases.
Our aim here is to help you find your footing and regain a sense of control. We'll explore what this internal battle means for day-to-day life and cover the essentials for building a resilient, fulfilling life.
- Symptom and Flare Management: Practical ways to handle daily discomfort and get through those intense periods when symptoms peak.
- Lifestyle Adjustments: How diet, exercise, and sleep can become your most powerful allies.
- Navigating Your World: Real-world advice on talking about your condition at work, with friends, and in your relationships.
- Mental and Emotional Wellbeing: Tackling the psychological side of things and building your mental resilience.
Your diagnosis is a significant chapter, but it doesn't get to define your entire story. You are still the author, and you have the power to shape the narrative through proactive management, self-compassion, and a great support system.
We're here to provide actionable advice and point you toward supportive resources that can genuinely improve your quality of life, one manageable step at a time. Your journey starts now.
Understanding What Happens Inside Your Body
To get a real handle on managing your health, it helps to understand what’s actually going on in your body, without needing a medical degree. Picture your immune system as a highly trained, incredibly diligent security team. Its main job is to patrol your body for genuine threats—like viruses, bacteria, and other invaders—and take them out to keep you safe.
Normally, this system is brilliant at telling the difference between 'friend' (your own cells) and 'foe' (harmful intruders). But with an autoimmune condition, something goes wrong with the communication. The security team gets bad intel and starts flagging your own healthy cells and tissues as dangerous enemies. In short, it’s a case of ‘friendly fire.’
This internal battle, where your body literally attacks itself, is what causes the inflammation and damage we see in over 100 different autoimmune diseases.
Organ Specific vs Systemic Conditions
Not all autoimmune attacks look the same. They can be incredibly targeted or much more widespread, and this difference is a huge factor in the kind of symptoms you might experience. We generally break them down into two main types.
- Organ-Specific Conditions: In these situations, the immune system’s attack is focused on one single organ. In Type 1 Diabetes, for example, the security team specifically goes after the insulin-producing cells in the pancreas. With Hashimoto's thyroiditis, the thyroid gland is the sole target.
- Systemic Conditions: This is where the attack is more generalised and can affect multiple organs and systems all over the body. Conditions like Lupus and Rheumatoid Arthritis fit in here, where the immune system can target anything from joints and skin to the kidneys and brain.
This distinction really helps explain why symptoms can be so wildly different from one person to the next. It all comes down to which part of your body is being mistakenly flagged as a threat.
The common thread running through every autoimmune disease is chronic inflammation. This isn't the helpful, short-term inflammation you get with a cut or sprain. It's a persistent, low-grade state of emergency that slowly wears the body down.
This constant inflammatory response is the direct cause of so many of the common symptoms. That profound, bone-deep fatigue you feel? That’s your body pouring enormous amounts of energy into this internal conflict. The joint pain, skin rashes, and digestive upset are all direct results of this relentless immune assault.
Understanding the Scale of Autoimmunity in the UK
If you’re feeling alone with your diagnosis, please know that you are part of a huge and growing community. It's estimated that over 3.5 million people in the UK are living with an autoimmune disease, with diagnoses rising steadily since the early 2000s. Psoriasis alone affects around 1.8 million people, while Inflammatory Bowel Disease (IBD) impacts over 550,000 of us. You can see more data on the UK’s growing autoimmune crisis on wecovr.com.
Living with this widespread inflammation often leads people to look deeper into how our different bodily systems are all connected. Many find it helpful to understand more about the body’s own regulatory networks. For instance, you can learn more about how the endocannabinoid system plays a key role in maintaining balance in our detailed guide. Getting to grips with the 'why' behind what you feel is a powerful first step in learning to better manage your life with an autoimmune disease.
Building Your Personal Management Toolkit
When you're living with an autoimmune disease, it helps to start thinking of yourself less as a patient and more as the CEO of your own health. A proactive, personal management plan is the single most powerful tool you have for navigating the twists and turns of your condition. It's about creating a structured, supportive framework for your life that truly listens to what your body needs.
This goes way beyond just showing up for appointments. It means working with your medical team, not just for them. It’s about understanding your treatment options inside and out, and then weaving that medical advice together with powerful lifestyle strategies that you control, day in and day out. This is how you get back in the driver's seat.
Assembling Your Medical Support Team
Your first move is to build a real partnership with your healthcare providers. This isn't a one-way street where you just get instructions; it's a collaboration. A typical team might include your GP alongside one or more specialists, like a rheumatologist if you're dealing with arthritis and systemic diseases, or a gastroenterologist for conditions such as Crohn's.
It’s so important to understand what each specialist does and what your medications are for. Treatments like immunosuppressants work by dialling down your immune system's overenthusiastic response, while biologics are a bit more targeted, blocking specific signals that fuel inflammation. Never be afraid to ask questions until you feel completely confident in your treatment plan.
The infographic below shows how autoimmune diseases are generally categorised, which often points to the type of specialist you might need to see.
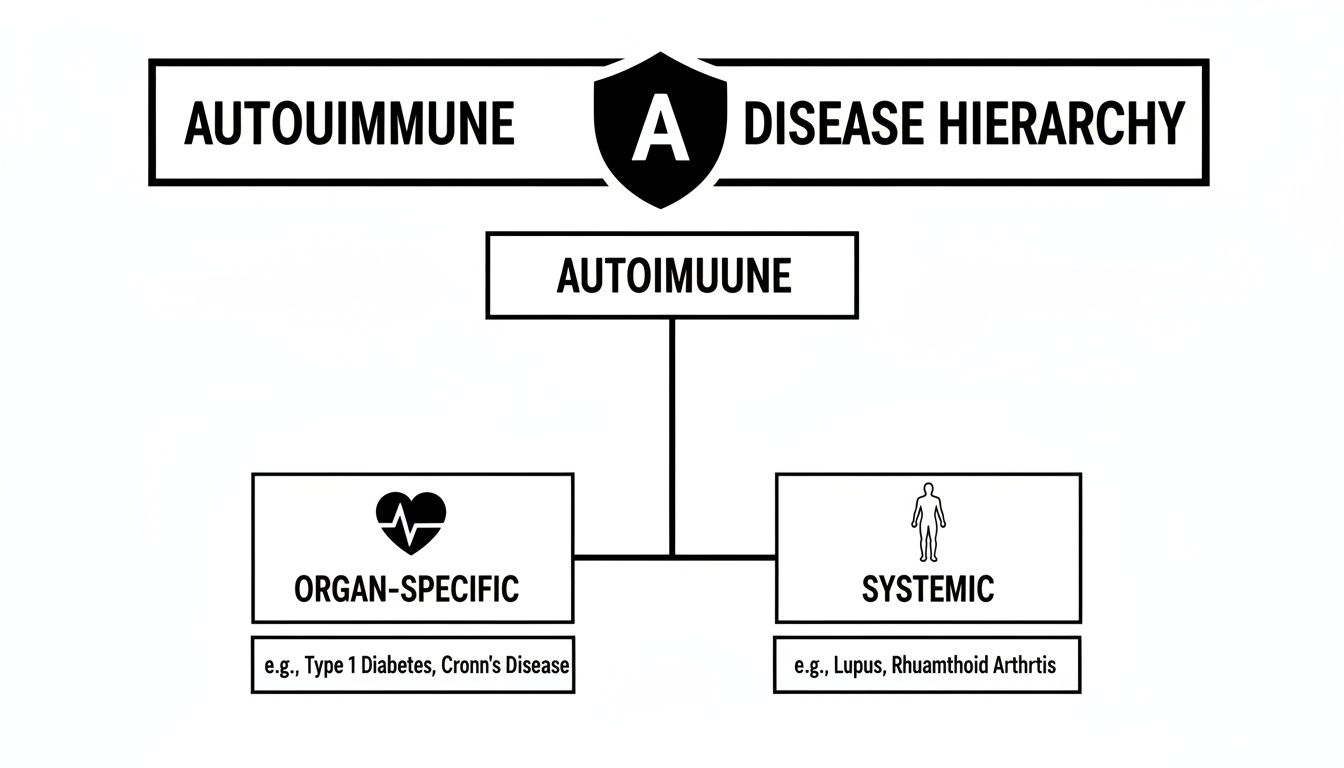
This visual helps make sense of whether a condition is mainly focused on one organ or affects systems all over the body, which is a key factor in how it's managed.
A solid, well-rounded management plan is your foundation for a better quality of life. The table below outlines the core pillars that can help you build a routine that supports your body and mind.
Core Pillars of an Autoimmune Management Plan
| Pillar | Focus Area | Example Actions |
|---|---|---|
| Medical Partnership | Collaborative Care | Regularly communicate with your GP and specialists. Ask questions about medications and treatments. |
| Pacing & Energy | Energy Management | Break down large tasks. Schedule mandatory rest periods. Learn to politely decline non-essential activities. |
| Nutrition | Anti-Inflammatory Diet | Focus on whole foods like oily fish, colourful vegetables, and healthy fats. Keep a food diary to spot triggers. |
| Sleep Hygiene | Restorative Rest | Aim for 7-9 hours of quality sleep. Create a relaxing bedtime routine (e.g., no screens, warm bath). |
| Gentle Movement | Joint-Friendly Exercise | Incorporate low-impact activities like walking, swimming, or gentle yoga into your weekly schedule. |
Building your daily life around these pillars isn't about restriction; it's about empowerment. Each one gives you another tool to help manage your symptoms and feel more in control.
Mastering the Art of Pacing
If there's one skill that can completely change the game, it's pacing. Think of your daily energy as a bank account with a very strict, unmovable limit. When you have a good day, it’s incredibly tempting to spend it all in one go, trying to catch up on everything you feel you've missed.
But that usually leads to a miserable 'boom-and-bust' cycle. You overdo it, which triggers a painful flare-up and forces you into days of bed-bound recovery. Pacing is all about spending that energy strategically. It means chopping up tasks into smaller, manageable chunks, building proper rest periods into your day, and getting comfortable with saying 'no' to protect your reserves.
Think of pacing not as a restriction, but as a smart investment. By spending your energy wisely today, you ensure you have enough for tomorrow, creating a more stable and predictable quality of life.
The Power of an Anti-Inflammatory Diet
While there’s no magic diet that can cure autoimmune disease, what you put on your plate can make a massive difference to your symptoms. The goal is to reduce chronic inflammation—the smouldering fire that drives so many of these conditions.
An anti-inflammatory way of eating is all about whole, unprocessed foods. This isn't about harsh restrictions; it’s about flooding your body with nutrients that help calm your immune system down.
Key Components of an Anti-Inflammatory Diet:
- Colourful Fruits and Vegetables: These are packed with antioxidants that help fight cellular damage.
- Oily Fish: Think salmon, mackerel, and sardines. They are rich in omega-3 fatty acids, which are powerful anti-inflammatory agents.
- Healthy Fats: You'll find these in avocados, olive oil, nuts, and seeds.
- Lean Proteins and Legumes: They provide the essential building blocks your body needs to repair itself.
On the flip side, it's a good idea to limit or avoid foods known to stoke inflammation, like heavily processed items, refined sugars, and too much red meat. Many people find keeping a food diary really helpful for identifying personal trigger foods that make them feel worse. Learning about the different ways you can reduce inflammation in the body can give you even more great ideas for your nutritional toolkit.
Prioritising Restorative Sleep and Gentle Movement
When you live with an autoimmune condition, sleep isn't a luxury. It's a non-negotiable part of your treatment plan. While you're in a deep sleep, your body is working overtime to repair tissues and regulate your immune function. Not getting enough quality sleep can ramp up inflammation and make you much more sensitive to pain.
Creating a calming bedtime routine can make a world of difference. This could be as simple as turning off all screens an hour before bed, taking a warm bath, or doing a few gentle stretches.
And what about exercise? It might sound like the last thing you want to do when you’re exhausted and in pain, but gentle movement is incredibly beneficial. The goal isn't to run a marathon; it's to find consistent, low-impact activity that feels good.
- Walking: A simple but brilliant way to keep your joints moving.
- Swimming or Water Aerobics: The water supports your joints, which makes movement feel so much easier and less painful.
- Yoga or Tai Chi: These practices are amazing because they combine gentle movement with mindfulness, helping to lower stress and improve flexibility at the same time.
Your personal management toolkit is a living, breathing thing. It's the combination of your medical treatments with these mindful lifestyle choices—pacing, nutrition, sleep, and movement—that creates a holistic strategy and puts you back in control.
Navigating Daily Life: Work and Relationships

An autoimmune disease isn't just a diagnosis you get from a doctor; it becomes a part of your daily life. It changes the game at work, reshapes your friendships and family dynamics, and most of all, it alters the relationship you have with yourself. Learning to handle these changes with a bit of self-kindness and clear communication is a huge part of living well with your condition.
That constant, low-level inflammation doesn’t just bring physical pain and exhaustion. It’s also deeply and undeniably tied to your mental health. This isn't something that's "all in your head"; it's a real, biological connection. Many of us find ourselves dealing with anxiety, depression, and that frustrating mental slowness often called "brain fog."
The mental strain is real. In fact, studies show that people with chronic inflammatory conditions have a much greater chance of developing depression. Just acknowledging that this link exists is the first, most important step you can take.
Protecting Your Mental Wellbeing
When your body is permanently in a state of high alert, your nervous system tends to get the memo and stay on edge, too. This can leave you feeling constantly anxious, frazzled, or just completely overwhelmed by the simplest things. It’s so important to find small, regular ways to help that internal alarm bell quieten down.
Things like mindfulness, simple breathing exercises, or even just taking five quiet minutes in the garden can make a surprising difference. If you're really struggling, remember that getting support through the NHS, like talking therapies, is a sign of true strength. For anyone curious about other methods, our guide on how to calm your nervous system has some gentle, practical ideas.
Managing Your Career and Workplace
For so many of us, our job is a big part of who we are, which makes trying to manage it with an unpredictable illness especially tough. The real trick is to stop trying to "push through" the bad days and start working smarter by standing up for what you need.
You do have rights. An autoimmune condition can be seen as a disability under the Equality Act 2010, which means your boss has a legal responsibility to make "reasonable adjustments" to help you.
Examples of Reasonable Adjustments:
- Flexible Hours: Starting a bit later or finishing earlier to work around morning stiffness or fatigue.
- Remote Work Options: The freedom to work from home on days when your symptoms are flaring up.
- Ergonomic Equipment: A proper supportive chair or an adjusted desk to ease physical strain.
- Location Adjustments: Moving your desk closer to the loos or kitchen to save precious energy.
Bringing this up with your manager can feel a bit scary. Try to frame it as a positive step to make sure you can keep doing your job well. Focus on the solutions, not just the problems.
Conversation Starter for Your Manager: "I'm really committed to my work here. To help me manage my health and stay productive, I'd like to chat about some small adjustments, like having a more flexible start time. I'm confident this would help me manage my energy and continue to do my best work for the team."
Nurturing Your Personal Relationships
An invisible illness can put a real strain on relationships with family and friends. From the outside, you might look perfectly "fine," which makes it incredibly difficult for them to grasp the battle you're fighting on the inside. This is especially true when you have to cancel plans at the last minute because a flare-up has hit.
Honest, open chats are your best friend here. Your loved ones aren't mind readers; they often want to support you but just don't know how. Explaining your limits isn't complaining – it's giving them a user manual on how to be there for you.
Using an analogy can work wonders. You could try explaining your energy using the "spoon theory," where you start each day with a limited number of spoons (energy units), and every single task, from showering to making breakfast, costs a spoon.
How to Explain Cancelling Plans:
- "I was so excited for tonight, but my symptoms have really hit me hard. I need to rest up so I can bounce back. Can we please reschedule for next week?"
- "Because of my condition, my energy levels are all over the place. Today is unfortunately a really low-energy day for me, so I won't be able to make it. I'm so sorry to let you down."
This way, they understand it’s about your health, not about them. It helps keep your relationships strong while you protect your own energy, which is absolutely vital when living with an autoimmune disease.
Finding Your Support System in the UK
Trying to navigate life with an autoimmune disease can feel incredibly lonely at times, but you absolutely do not have to walk this path by yourself. Building a solid support network isn't a sign of weakness; it’s one of the smartest things you can do to build resilience and improve your day-to-day life. Think of it as putting together your own personal team—a group of people dedicated to helping you thrive.
There's something incredibly powerful about connecting with others who genuinely understand the daily grind of fatigue, pain, and unpredictability. It creates a space where you don't have to constantly explain yourself or put on a brave face when you're just not feeling it. This is all about finding your tribe—a mix of medical experts, trusted friends, family, and other people who just get it.
Trusted UK Charities and Organisations
The UK has some fantastic organisations that provide brilliant resources, from telephone helplines staffed by trained advisors to funding for vital research. These charities are often the best first stop for reliable, condition-specific information and a sense of community.
- Versus Arthritis: An essential resource for anyone living with arthritis and related conditions. They offer a huge amount of information on managing pain, understanding treatment options, and finding local support groups across the country.
- The Lupus Trust: Focussing specifically on lupus, this trust works hard to improve diagnosis and treatment through its research, particularly at St Thomas' Hospital.
- Crohn's & Colitis UK: The leading charity for inflammatory bowel disease (IBD) in the UK. They provide confidential support lines, practical guides, and a strong community for people affected by Crohn's and ulcerative colitis.
These organisations know all too well the growing burden these conditions place on people and the NHS. The rising number of people living with autoimmune disease is creating huge challenges, with some estimates suggesting certain conditions could lead to lifetime healthcare and societal costs of over £4 million per person. You can read more about these UK autoimmune disease statistics and their impact on the NHS.
The Power of Peer Support
While expert advice from your doctor is crucial, there’s a unique kind of magic in talking to someone who is on a similar journey. Peer support—connecting with others who have the same or a similar diagnosis—can massively reduce feelings of isolation and offer practical, lived-in tips you simply won't find in a medical textbook.
These connections can happen in all sorts of ways. You might find a local group that meets for a coffee, or you might prefer the convenience of an online forum or a private social media group. The most important thing is finding a community that feels safe, supportive, and is well-moderated.
Finding a support group is like finding a shortcut to understanding. It's a space where your experiences are immediately valid, and the shared wisdom can help you navigate challenges you thought you were facing alone.
As you explore these groups, you’ll probably find that conversations about complementary approaches pop up. Many people share what’s worked for them, including different wellness products like CBD. If this is something you're curious about, it’s a good idea to stay informed on the rules. Our guide offers a clear overview, helping you understand UK CBD law and compliance requirements.
Building your support system is a powerful, proactive step. It means that on the tough days, you have a network ready to offer a helping hand, sensible advice, and most importantly, real understanding.
Frequently Asked Questions
Living with an autoimmune condition means you're constantly learning and adapting. It's completely normal to have questions pop up along the way. Here are some straightforward answers to the things people ask most often.
Can Diet Really Make a Difference?
Absolutely. While there's no magic diet that will cure an autoimmune disease, what you eat can play a massive role in how you feel day-to-day. Many people find significant relief by adopting an anti-inflammatory way of eating. This isn't about restriction; it's about focusing on whole, nourishing foods like colourful vegetables, oily fish, lean proteins, and healthy fats while dialling back on processed foods and refined sugars.
Some people also discover they have personal food triggers, like gluten or dairy, that make their symptoms worse. A great way to figure this out is by keeping a simple food diary to see if you can spot any patterns. Just remember, it's always a good idea to chat with your GP or a registered dietitian before making any big changes to make sure you're still getting all the nutrients your body needs.
How Do I Explain My Invisible Illness?
This is one of the hardest parts, without a doubt. It can be incredibly frustrating to look fine on the outside while feeling awful on the inside. Being direct but simple is often the best approach. You might say something like, "Even though I look okay, my immune system is attacking my body, which leaves me with a lot of pain and fatigue."
Analogies can be your best friend here. Comparing your daily energy to a phone battery that starts at 50% and drains incredibly fast can really help people grasp the concept. It's also okay to set boundaries. Explaining that you have to cancel plans isn't a reflection on them, but a necessary act of self-preservation.
"A flare is a temporary period when the symptoms of your autoimmune disease suddenly worsen. It's crucial to remember that a flare is part of the disease process, not a personal failure."
What Is a Flare and How Can I Manage It?
A ‘flare’ is basically when your symptoms decide to throw a massive, unwelcome party. Disease activity spikes, and you feel much worse. This can be triggered by anything from stress and lack of sleep to picking up a common cold. The first step is to follow the flare plan you've made with your doctor, which might mean tweaking your medication for a short time.
When you're in a flare, rest isn't a luxury; it's non-negotiable. This is when your pacing skills become your superpower. You have to dial everything back – physically and mentally. Gentle stress-reducers can also be a huge help, whether that's some deep breathing exercises or just putting on some calming music. Most of all, give yourself some grace.
At SMOKO CBD, we're here to support your wellness journey with high-quality, UK-made CBD products that can help with managing pain, getting better sleep, and finding a bit of calm in the chaos. Take a look at our lab-tested CBD oils and edibles to see if they might be right for you.









