Living with arthritis often feels like a daily battle against pain, stiffness, and inflammation. While medications and therapies play a crucial role, a powerful and often overlooked ally in this fight is your diet. The food you eat can either fuel the inflammatory fire or help to extinguish it, making your daily choices at the dinner table incredibly impactful.
Many common foods, including some you might consider harmless, contain compounds that can trigger inflammatory responses. This can lead to painful flare-ups and a worsening of joint symptoms over time. Understanding these dietary triggers is the first, most crucial step toward regaining a sense of control over your condition and daily comfort levels. This guide is designed to empower you with that knowledge.
We will uncover the top eight arthritis foods to avoid, delving into the science behind why they can cause problems for your joints. More importantly, we will provide practical, actionable advice and suggest delicious alternatives for each category. By making strategic and informed changes to your shopping list, you can begin to transform your meals from a source of potential pain into a powerful tool for achieving lasting relief and promoting better long-term joint health.
1. Refined Sugars and High-Sugar Foods
Refined sugars, frequently found in fizzy drinks, sweets, pastries, and many processed foods, are a significant contributor to inflammation throughout the body. When you consume these sugars, your body responds by releasing inflammatory messengers known as cytokines. This process can directly intensify the symptoms of arthritis, including joint pain, swelling, and stiffness.
This inflammatory cascade is further amplified by the creation of advanced glycation end products (AGEs). AGEs form when protein or fat combines with sugar in your bloodstream, and high levels of these compounds can promote oxidative stress and inflammation, damaging joint cartilage over time. Research consistently links high sugar consumption with negative arthritis outcomes; a study in The American Journal of Clinical Nutrition found that women who drank one or more sugary drinks daily had an increased risk of developing rheumatoid arthritis.
How Sugar Triggers Arthritis Flares
The connection between sugar and joint pain isn't just theoretical; it's a measurable biological process. A rapid increase in blood glucose from sugary foods prompts an inflammatory response that can make sensitive joints feel worse. For many, this translates into more painful and stiff mornings or increased discomfort after a high-sugar meal.
The infographic below summarises the direct impact of refined sugars on the body’s inflammatory processes.
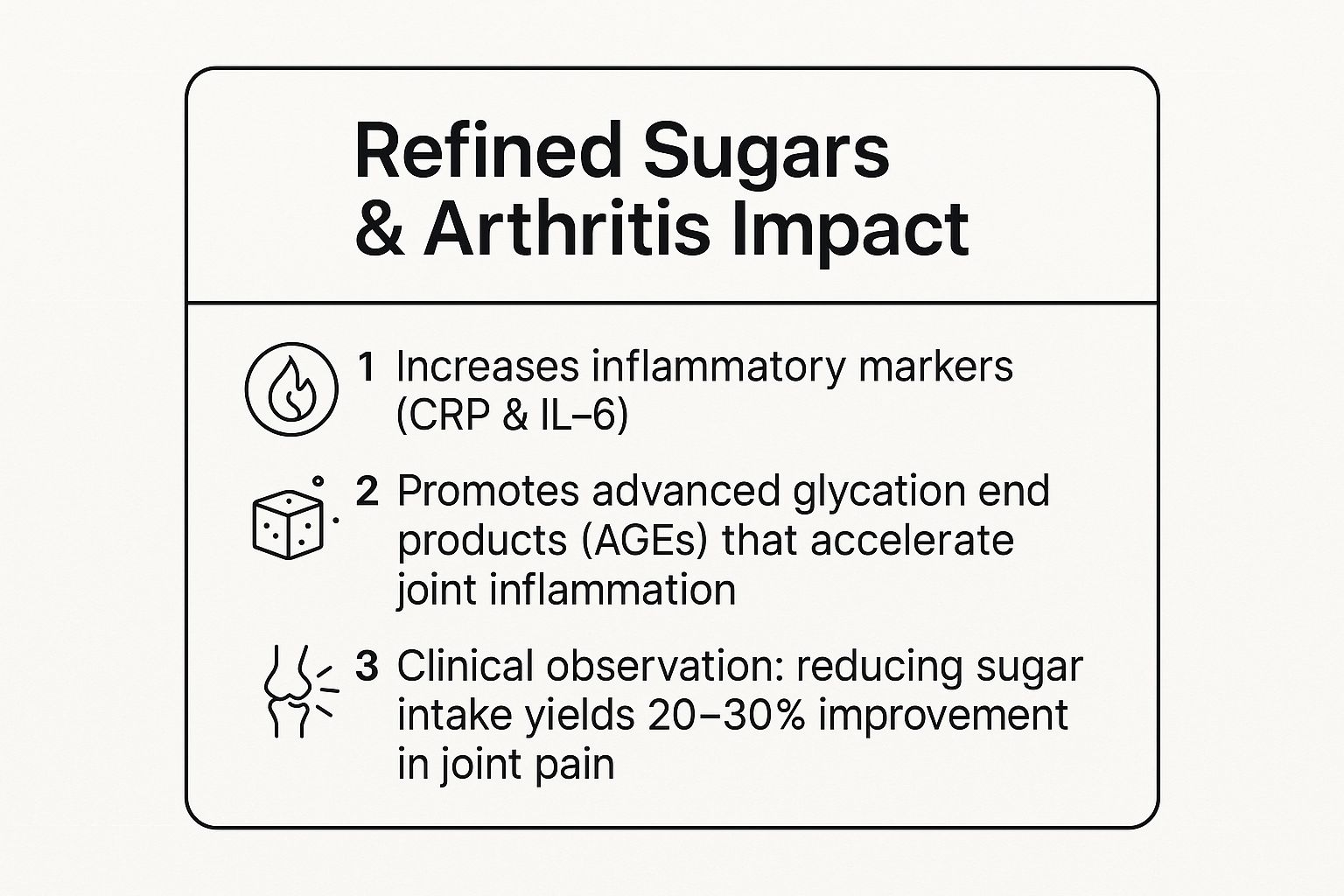
This data highlights how sugar directly promotes inflammation markers and AGEs, while also showing the tangible benefits of reducing your intake.
Actionable Tips for Reducing Sugar
Making changes can feel daunting, but small, consistent steps are key to managing your intake and, in turn, your arthritis symptoms. Consider these practical strategies:
- Read nutrition labels carefully. Sugar hides under many names, such as sucrose, high-fructose corn syrup, and dextrose. Be vigilant about checking ingredients lists on packaged foods.
- Swap sugary drinks. Replace fizzy drinks and cordials with water infused with lemon, mint, or berries. Herbal teas are another excellent, flavourful alternative.
- Choose whole foods. Opt for whole fruits instead of fruit juices or dried fruits, which have a much higher concentration of sugar.
- Track your intake and symptoms. Keep a food diary to identify correlations between what you eat and how your joints feel. This can be a powerful motivator to make lasting changes.
By actively reducing refined sugars, you can take a significant step towards managing your inflammation. If you're exploring complementary approaches, you can learn more about how to manage inflammation throughout your body on smokocbd.com.
2. Processed and Red Meats
Processed meats like bacon, sausages, and deli slices, along with excessive consumption of red meats such as beef and lamb, are often linked to heightened inflammation. These foods are typically high in saturated fats and omega-6 fatty acids, which can disrupt the body's natural inflammatory balance and worsen arthritis symptoms. They are also significant sources of advanced glycation end products (AGEs), compounds that promote oxidative stress and joint damage.
The preservatives used in many processed meats, such as nitrites and nitrates, can further contribute to the body's inflammatory load. Studies support this connection; for instance, research published in Arthritis Care & Research found that higher red meat intake correlated with increased disease activity in people with rheumatoid arthritis. Similarly, clinical trials have shown that reducing red meat to just once weekly can improve arthritis symptoms in a significant percentage of patients.
How These Meats Worsen Joint Pain
The pro-inflammatory compounds in processed and red meats can directly aggravate the sensitive tissues in your joints. When your body breaks down these foods, it can trigger the release of inflammatory cytokines, the same messengers involved in the arthritis disease process. This reaction can lead to increased joint pain, swelling, and morning stiffness, making it one of the key arthritis foods to avoid for symptom management.
Actionable Tips for Reducing Your Intake
Swapping out processed and red meats can be a powerful step towards feeling better. These practical strategies can help you make a smooth transition:
- Limit red meat consumption. Aim to have red meat no more than once a week. This simple change can make a noticeable difference in your inflammatory levels.
- Prioritise lean proteins. Choose lean poultry, fish, or plant-based proteins like beans, lentils, and tofu as your primary protein sources.
- Choose grass-fed options. If you do eat red meat, opt for grass-fed varieties, which typically have a more favourable omega-3 to omega-6 fatty acid profile.
- Adopt 'Meatless Mondays'. Dedicating one day a week to plant-based meals is an easy way to gradually reduce your overall consumption and explore new recipes.
- Opt for omega-3 rich fish. Replace red meat with cold-water fish like salmon, mackerel, and sardines, which are rich in anti-inflammatory omega-3 fatty acids.
3. Gluten-Containing Grains (for sensitive individuals)
Gluten, a protein found in wheat, barley, and rye, can be a potent inflammatory trigger for certain individuals. While strongly associated with coeliac disease, a growing body of evidence suggests a connection between gluten sensitivity and exacerbated arthritis symptoms. For susceptible people, consuming gluten can provoke an immune response that starts in the gut but leads to systemic inflammation, directly impacting sensitive joints.
This process is often linked to increased intestinal permeability, sometimes called 'leaky gut'. When the gut lining is compromised, undigested gluten proteins can enter the bloodstream, prompting an immune reaction that can worsen joint pain, swelling, and stiffness. Research highlights this link; a study in Rheumatology International found that 41% of rheumatoid arthritis patients reported significant improvement on a gluten-free diet. This makes understanding your personal tolerance to these grains a crucial step in managing arthritis.
How Gluten Can Trigger Arthritis Flares
For individuals with a sensitivity, the link between gluten and joint pain is driven by the body's immune system mistakenly identifying gluten proteins as a threat. This sets off an inflammatory cascade that isn't confined to the digestive system. The resulting inflammation can travel throughout the body, settling in the joints and intensifying the chronic pain and discomfort characteristic of arthritis.
This is particularly relevant for those with autoimmune forms of arthritis, like rheumatoid or psoriatic arthritis, as their immune systems are already primed to overreact. Case studies have shown patients with psoriatic arthritis experiencing dramatic symptom reduction after eliminating gluten, demonstrating a powerful, personalised connection.
Actionable Tips for Assessing Gluten Sensitivity
Determining if gluten is one of the foods to avoid for your arthritis requires a systematic approach. Consider these practical strategies to see if a gluten-free diet is right for you:
- Conduct a 30-day elimination trial. Remove all sources of gluten from your diet for a month, keeping a detailed symptom diary to track any changes in joint pain, stiffness, or energy levels.
- Read labels meticulously. Gluten is often hidden in unexpected products like soy sauce, salad dressings, soups, and even some medications. Always check the ingredients list.
- Choose naturally gluten-free grains. Swap wheat, barley, and rye for whole-grain alternatives like quinoa, brown rice, millet, and buckwheat to maintain a balanced intake of fibre and nutrients.
- Test for coeliac disease first. Before starting an elimination diet, it's wise to get tested for coeliac disease to ensure an accurate diagnosis, as going gluten-free can affect test results.
By carefully evaluating your body's response, you can determine if gluten is a contributing factor to your inflammation. As you explore dietary changes, you can also learn how CBD oil may help treat arthritis as part of a comprehensive management plan.
4. Omega-6 Rich Vegetable Oils
Common cooking oils like corn, sunflower, safflower, and soybean oil are extremely high in omega-6 fatty acids. While your body needs omega-6s, the modern Western diet provides them in excessive amounts, creating a significant imbalance with anti-inflammatory omega-3 fatty acids. This skewed ratio, often as high as 20:1 instead of the ideal 4:1, promotes the production of pro-inflammatory eicosanoids, directly worsening arthritis symptoms like pain and swelling.
This imbalance is a key reason why certain oils are considered arthritis foods to avoid. An overabundance of omega-6 fatty acids can accelerate joint damage by maintaining a constant state of low-grade inflammation. Research highlights this connection; a study in the Journal of Nutrition and Metabolism demonstrated that reducing omega-6 intake from vegetable oils led to a significant decrease in arthritis pain scores over just 12 weeks. Clinical trials have also shown that replacing these oils with omega-3 rich alternatives measurably reduces inflammatory markers in the blood.
How an Omega-6 Imbalance Triggers Arthritis Flares
The link between these vegetable oils and arthritis pain is rooted in biochemistry. When the omega-6 to omega-3 ratio is too high, your body's inflammatory pathways become overactive. This can lead to increased joint tenderness, more frequent flare-ups, and a general feeling of stiffness, particularly after consuming meals prepared with these common cooking oils found in processed foods and many restaurant meals.
Actionable Tips for Balancing Your Fats
Correcting this fatty acid imbalance is a powerful strategy for managing arthritis symptoms. Small adjustments to your cooking and shopping habits can make a significant difference.
- Choose your cooking oils wisely. Use extra virgin olive oil for low-heat cooking and dressings. For high-heat cooking, opt for avocado oil or coconut oil.
- Read ingredient labels. Many processed foods, from biscuits to ready meals, contain high levels of soybean, corn, or sunflower oil. Be vigilant and choose products that avoid them.
- Make your own dressings. Shop-bought salad dressings are often based on omega-6 rich oils. Create simple, healthier versions at home using extra virgin olive oil, lemon juice, and herbs.
- Boost your omega-3 intake. Actively increase your consumption of omega-3s from sources like fatty fish (salmon, mackerel), flaxseed, and chia seeds to help restore a healthier fatty acid ratio.
5. Fried and Deep-Fried Foods
Foods cooked at high temperatures, such as those deep-fried or pan-fried in oil, undergo chemical changes that create highly inflammatory compounds. This category includes popular items like chips, fried chicken, doughnuts, and battered fish, which are known to trigger inflammatory pathways that can worsen arthritis symptoms. The high-heat cooking process generates advanced glycation end products (AGEs) and trans fats, both of which are strongly linked to increased inflammation and oxidative stress in the body.
Furthermore, many fried foods are cooked in omega-6-rich vegetable oils, such as corn or sunflower oil. While some omega-6 is necessary, an excessive intake, especially when unbalanced with omega-3 fatty acids, can promote the production of pro-inflammatory chemicals. This issue is often compounded in commercial kitchens where oils are reused multiple times, concentrating these harmful compounds and making the final product even more inflammatory.

How Frying Triggers Arthritis Flares
The link between fried foods and arthritis pain is well-documented. Research from the Mount Sinai School of Medicine found that when people reduced their intake of fried and processed foods, levels of inflammatory markers in their bodies decreased significantly. For someone with arthritis, consuming these foods can lead to a direct increase in joint pain, stiffness, and swelling. Many patients report a noticeable improvement in their symptoms within just a few weeks of eliminating fried items from their diet.
This video explores the connection between diet and joint health in more detail.
Actionable Tips for Reducing Fried Foods
Avoiding fried foods doesn't mean giving up on flavour or texture. With a few simple adjustments, you can enjoy delicious meals that support your joint health. Consider these practical alternatives:
- Use an air fryer. This popular kitchen appliance circulates hot air to create a crispy texture similar to deep-frying but with a fraction of the oil.
- Bake or roast instead. Try baking "fries" or chicken pieces in the oven with a light spray of olive oil and a generous amount of herbs and spices for flavour.
- Be mindful when dining out. Most restaurants offer grilled, baked, or steamed options. Don't hesitate to ask for your food to be prepared using one of these healthier methods.
- Read labels on packaged snacks. Many crisps, crackers, and pre-made meals are fried. Look for products that are explicitly baked or air-popped.
Making these changes can significantly lower your body's inflammatory load. If you are struggling with localised joint discomfort, you can get insights into managing arthritis finger pain relief on smokocbd.com.
6. Refined Carbohydrates and White Flour Products
Refined carbohydrates, such as white bread, white pasta, pastries, and crackers, have been processed in a way that strips them of their beneficial fibre, vitamins, and minerals. This not only diminishes their nutritional value but also makes them a key trigger for inflammation. Because they are easily broken down, these foods cause a rapid spike in blood glucose, prompting the body to release a flood of inflammatory messengers.
This process is directly linked to the exacerbation of arthritis symptoms. Foods with a high glycaemic index, like white flour products, are quickly converted into sugar in your bloodstream. This contributes to the formation of advanced glycation end products (AGEs), which are known to promote oxidative stress and degrade joint cartilage. Research supports this link; one study found that switching from refined to whole grains significantly reduced C-reactive protein (CRP), a key inflammatory marker, showcasing how influential this dietary change can be for those managing arthritis.
How Refined Carbs Worsen Joint Pain
The immediate effect of consuming refined carbohydrates is an increase in blood sugar and insulin, which sets off a pro-inflammatory cascade. For someone with arthritis, this can translate directly into heightened joint pain, increased swelling, and more pronounced morning stiffness. The body essentially reacts to these foods as it would to an injury, mobilising an inflammatory response that targets already sensitive joints.
Many people with arthritis report a noticeable improvement in their mobility and a reduction in pain after consciously removing white flour and other refined carbs from their diet. This makes managing carbohydrate quality one of the most effective dietary strategies for controlling symptoms.
Actionable Tips for Reducing Refined Carbs
Swapping out refined carbohydrates doesn't have to be difficult. Focusing on whole, unprocessed alternatives can make a significant difference in your joint health and overall well-being.
- Choose whole grains. Replace white bread with 100% wholemeal or sprouted grain bread. Opt for brown or wild rice and quinoa instead of white rice.
- Read ingredient labels. Be wary of terms like "wheat flour," which is often just refined flour. Look for "whole wheat" or "whole grain" as the first ingredient to ensure you're getting the full benefit.
- Rethink your pasta. Try whole wheat pasta or explore alternatives made from legumes like chickpeas or lentils, which offer more fibre and protein.
- Balance your meals. When you do eat carbohydrates, pair them with a source of protein and healthy fat to slow down sugar absorption and prevent sharp blood glucose spikes.
7. Alcohol (Excessive Consumption)
While a single glass of wine may seem harmless, excessive alcohol consumption is known to promote inflammation and can significantly worsen arthritis symptoms. Alcohol places a direct strain on the body's systems, particularly the liver, which is crucial for filtering inflammatory compounds. When its function is compromised, inflammation can increase, leading to more pronounced joint pain, swelling, and stiffness for those with arthritis.
Furthermore, alcohol can increase intestinal permeability, a condition often referred to as 'leaky gut'. This allows bacterial toxins to pass from the gut into the bloodstream, triggering a systemic inflammatory response that can directly impact sensitive joints. A study published in Arthritis Research & Therapy highlighted that moderate to heavy alcohol consumption was associated with increased severity in rheumatoid arthritis patients. For those with gout, beer is especially problematic due to its high purine content, which is strongly linked to flare-ups.
How Alcohol Triggers Arthritis Flares
The link between alcohol and joint pain is multifaceted. Beyond its direct inflammatory effects, alcohol can disrupt sleep patterns, and poor sleep is a well-known trigger for increased pain perception and inflammation. It also depletes the body of essential nutrients needed for joint health and can interfere with the effectiveness and safety of common arthritis medications, including non-steroidal anti-inflammatory drugs (NSAIDs) and methotrexate. This chemical interaction not only reduces the medication's benefit but also increases the risk of side effects.
Actionable Tips for Reducing Alcohol
Managing your alcohol intake is a practical and effective way to help control arthritis symptoms. Making mindful choices can lead to a noticeable reduction in flare-ups.
- Limit your intake. Aim to reduce consumption to occasional use, such as one or two drinks per week, rather than several drinks in one sitting.
- Choose wisely. If you do drink, consider a small glass of red wine, which contains the antioxidant resveratrol. Try to avoid beer if you have gout or gluten sensitivity.
- Stay hydrated. Drink a glass of water for every alcoholic beverage consumed to help your liver process the alcohol and stay hydrated.
- Check with your doctor. Never mix alcohol with arthritis medications without first consulting your doctor to understand the potential risks and interactions.
- Track your symptoms. Keep a diary to note any correlation between your alcohol consumption and the severity of your joint pain. Recognising this pattern can be a powerful motivator.
8. Salt and High-Sodium Processed Foods
Excessive sodium from table salt and highly processed foods is a key trigger for inflammation and can significantly worsen arthritis symptoms, particularly rheumatoid arthritis. High sodium intake can activate specific inflammatory immune cells, leading to a pro-inflammatory state. It also causes the body to retain water, which increases fluid pressure within the joints and can lead to heightened pain and swelling.
The link between salt and arthritis is supported by growing evidence. Research in the Journal of Clinical Investigation found that a high-salt diet increased the number of inflammatory Th17 cells, which are strongly associated with autoimmune conditions like rheumatoid arthritis. The majority of dietary sodium comes not from the salt shaker but from processed foods, including canned goods, ready meals, cured meats, and packaged snacks, where it is used extensively as a preservative and flavour enhancer.
How Salt Triggers Arthritis Flares
The connection between high sodium intake and joint pain is a direct physiological process. When you consume too much salt, your body's immune system can be thrown off balance, favouring inflammatory responses that target sensitive joints. This can manifest as increased morning stiffness, more pronounced swelling, and a general worsening of daily discomfort. Clinical observations have shown that reducing daily sodium intake below 2,000mg can lead to a noticeable decrease in joint swelling for a significant number of patients.
Actionable Tips for Reducing Salt
Managing your sodium intake is a powerful strategy for controlling inflammation. Small adjustments to your diet can make a substantial difference in how your joints feel.
- Read nutrition labels. Always check the sodium content on packaged foods. Aim for products with less than 140mg of sodium per serving, which is considered low-sodium.
- Cook from scratch. Preparing meals at home with fresh ingredients gives you complete control over how much salt is added.
- Flavour with alternatives. Replace salt with herbs, spices, garlic, onion powder, lemon juice, or vinegar to add flavour to your dishes without the sodium.
- Rinse canned goods. Rinsing canned beans, lentils, and vegetables under running water can wash away up to 40% of the added sodium.
- Be mindful when eating out. Restaurant and takeaway meals are often extremely high in sodium. Ask for your meal to be prepared with less salt or for sauces to be served on the side.
By consciously lowering your sodium consumption, you can help manage the inflammatory processes driving your arthritis. For those interested in a broader approach, you can find more information about natural relief strategies for inflammation at smokocbd.com.
Arthritis Foods to Avoid: Top 8 Comparison
| Item | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Refined Sugars and High-Sugar Foods | Moderate - requires label reading and gradual reduction | Low - mainly behavioural changes and food swaps | Reduced inflammation and joint pain 20-30% improvement | Arthritis patients sensitive to sugar and inflammation | Breaks inflammatory cycle, improves pain quickly |
| Processed and Red Meats | Moderate - requires dietary substitutions and cooking changes | Moderate - sourcing lean/alternative proteins | Lower arthritis activity and joint pain reduction | Patients with RA and gout risk | Reduces purine and AGE intake, improves inflammation |
| Gluten-Containing Grains (sensitive individuals) | Variable - needs testing and strict elimination trial | Moderate - gluten-free alternatives can be costly | Improvement in autoimmune-related arthritis symptoms | Those with gluten sensitivity, celiac, or RA subtypes | Helps reduce systemic and intestinal inflammation |
| Omega-6 Rich Vegetable Oils | Moderate - replacement of cooking oils and label vigilance | Low to moderate - purchasing alternative oils | Significant decrease in inflammatory markers | Patients with chronic arthritis and inflammation | Balances fatty acid ratio, reduces pro-inflammatory eicosanoids |
| Fried and Deep-Fried Foods | High - requires major cooking method changes and avoidance of fast food | Moderate - requires new cooking tools or options | Up to 75% reduction in inflammation, symptom improvement | Those consuming frequent fried/fast foods | Eliminates highest AGE sources and oxidized fats |
| Refined Carbohydrates and White Flour Products | Moderate - dietary swap to whole grains, label reading | Low - common whole grain alternatives widely available | Decreased inflammatory markers, better joint function | Patients sensitive to blood sugar spikes and insulin | Improves glycemic control, reduces cytokine production |
| Alcohol (Excessive Consumption) | High - requires strict intake control and medication awareness | Low - mainly behavioural with occasional substitutions | Reduced inflammatory cytokines and improved medication efficacy | Arthritis patients on medications or with gout | Limits nutrient depletion and leaky gut effects |
| Salt and High-Sodium Processed Foods | Moderate - careful label reading, cooking adjustments | Low - use of herbs/spices and fresh ingredients | Lower joint swelling and reduced autoimmune activity | Patients with RA and high blood pressure | Reduces fluid retention and immune activation |
Taking Control: Building Your Anti-Inflammatory Eating Plan
Navigating the world of nutrition can feel overwhelming, especially when you're trying to manage a condition like arthritis. However, understanding which foods can potentially worsen inflammation is a powerful first step towards reclaiming control over your joint health. This guide has detailed the primary culprits, from the processed sugars in your favourite snacks to the high levels of omega-6 fatty acids found in certain vegetable oils and the pro-inflammatory compounds in red and processed meats.
The core message is not one of deprivation, but of mindful substitution. By identifying these potential triggers, you empower yourself to make smarter, more beneficial choices that actively support your body's efforts to reduce inflammation. The journey to managing arthritis symptoms is highly personal, and what works for one person may not work for another. This is where self-awareness becomes your greatest tool.
Your Personalised Path to Relief
The true value in understanding arthritis foods to avoid lies in creating a sustainable, long-term eating strategy. This isn't about a restrictive diet; it's about building a foundation of nourishment. The goal is to shift the balance on your plate away from pro-inflammatory items and towards foods that soothe and protect.
Key takeaways to implement immediately include:
- Focus on Addition, Not Just Subtraction: Instead of dwelling on what you're removing, concentrate on what you can add. Think vibrant, colourful vegetables, antioxidant-rich berries, omega-3-packed fish like salmon and mackerel, and healthy fats from avocados, nuts, and seeds.
- Become a Label Detective: Start consciously reading food labels. Pay close attention to added sugars, sodium content, and the types of oils used in processed foods. This simple habit can reveal hidden sources of inflammation in your everyday diet.
- Listen to Your Body: Consider keeping a food and symptom diary for a few weeks. Note what you eat and how your joints feel afterwards. This practice can help you identify personal food sensitivities that might not be on a generic list, offering invaluable insight into your unique triggers.
A Holistic Approach to Wellbeing
Mastering your diet is a cornerstone of arthritis management, but it's most effective when integrated into a broader, holistic wellness plan. By combining an anti-inflammatory eating pattern with other supportive habits, you create a powerful synergy that can lead to more significant and lasting relief. Think of it as building a comprehensive defence system for your joints.
This broader approach might include gentle, joint-friendly exercise like swimming or yoga, stress-management techniques such as mindfulness or meditation, and ensuring you get adequate, restorative sleep. It’s about nurturing your entire body, not just focusing on your joints in isolation. By adopting this well-rounded strategy, you're not just fighting inflammation; you're actively promoting overall health, vitality, and resilience, which enhances your quality of life far beyond symptom management.
For those seeking to complement their dietary efforts with natural wellness solutions, exploring the benefits of high-quality CBD can be a valuable next step. Many people with joint discomfort incorporate CBD into their daily routine to help manage pain and support their body’s balance due to evidence that CBD can help attenuate the inflammatory response and may positively impact pain perception.
Discover the premium, lab-tested range of CBD oils and edibles at SMOKO CBD and see how they can support your journey to better joint health.









